
With the Dexcom CGM System, see your glucose numbers without fingersticks.*
Nick Jonas, Paid spokesperson of Dexcom, Inc.
* Fingersticks required for diabetes treatment decisions if symptoms or expectations do not match readings.
What is a continuous glucose monitoring (CGM) device?
A continuous glucose monitoring (CGM) device tracks glucose levels throughout the day and night and can alert you if your levels go too low or when you’re high. It measures your glucose level at regular intervals, as frequently as every 5 minutes, and translates the readings into easy-to-read data and insights. It can also show the direction your glucose is heading and how fast.
Better diabetes management with a Dexcom CGM System
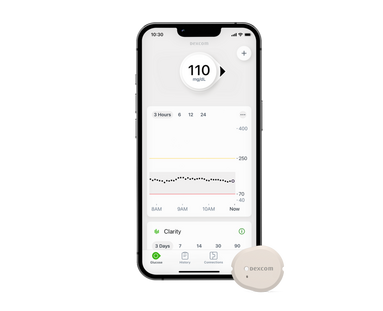
A Dexcom CGM system is an FDA-cleared wearable device that tracks your glucose levels continuously throughout the day and night. Your glucose reading is sent to your smartphone, smart device† or receiver as frequently as every five minutes. Dexcom CGM systems then translate your readings into dynamic data so you're better able to manage your diabetes treatment.

Glucose at a glance for more informed decisions
See your glucose numbers right on your smart device† or receiver without fingersticks. You can even see the direction your glucose is heading – up, down, or steady, so you can make better decisions about food, activity, and insulin in the moment. With Dexcom CGM, there’s no more guessing, making diabetes management easier.*
* Fingersticks required for diabetes treatment decisions if symptoms or expectations do not match readings.
How does a continuous glucose monitoring system work?
Instead of looking at one glucose number at a single moment in time, a CGM system tracks your glucose levels day and night. Here's how:

1. Easy, painless application1
Users insert a slim sensor wire under their skin using an automatic applicator. An adhesive patch holds the CGM device in place so it can measure glucose readings in interstitial fluid 24/7.

2. Small, discreet wearable
A small, reusable transmitter connects to the sensor wire and sends real-time readings automatically to a smart device† or receiver so you can view your numbers without fingersticks.*
* Fingersticks required for diabetes treatment decisions if symptoms or expectations do not match readings.

3. Real-time numbers & alerts
The compatible smart device† displays current glucose levels, as well as historical trends. Set customizable alerts that can warn you of highs and lows.

CGM systems can help you lower your A1C2-6
Studies have shown that use of some CGM systems may help reduce A1C levels and reduce risk of hypoglycemia, whether users are on insulin injections or pump therapy.7

Discover how the Dexcom CGM System can fit into your lifestyle
- No more fingersticks*
- Glucose numbers at a glance
- Easy to use8
- Customizable high & low alerts
- Daily event logs to track food, activity, and insulin
- Up to 10 people can follow‡ your glucose numbers
*Fingersticks required for diabetes treatment decisions if symptoms or expectations do not match readings.
Learn more about Dexcom CGM Systems
Watch and learn more about the value and benefits of CGM.
How Dexcom CGM works
The benefits of Dexcom CGM
8 reasons to get Dexcom CGM

Get started with Dexcom G7
If you are a new Dexcom user, fill out the Get Started form to get a free benefits check.
If you are a current Dexcom G6 user, please speak to your doctor about getting a prescription for Dexcom G7. Check out the FAQ for further details
*If your glucose alerts and readings from your CGM do not match symptoms or expectations, use a blood glucose meter to make your diabetes treatment decisions. †For a list of compatible devices, visit https://www.dexcom.com/compatibility‡ Separate Follow app and internet connection required.
1 Shah VN, et al. Diabetes Technol Ther. 2018;20(6):428-433. 2 Beck, RW, et al. JAMA. 2017;317(4):371-378. 3 Beck RW, et al. Ann Intern Med. 2017;167(6):365-374. 4 Martens T, et al. JAMA. 2021;325(22):2262-2272. 5 Laffel LM, et al. JAMA. 2020;323(23):2388-2396. 6 Welsh JB, et al. J Diabetes Sci Technol. 2022:19322968221099879. 7 Soupal J, Petruzelkova L, Grunberger G, et al. Diabetes Care 2019;43(1):37-43. 8 Dexcom, data on file, 2020.
BRIEF SAFETY STATEMENT Failure to use the Dexcom G6 Continuous Glucose Monitoring System (G6) and its components according to the instructions for use provided with your device and available at https://www.dexcom.com/safety-information and to properly consider all indications, contraindications, warnings, precautions, and cautions in those instructions for use may result in you missing a severe hypoglycemia (low blood glucose) or hyperglycemia (high blood glucose) occurrence and/or making a treatment decision that may result in injury. If your glucose alerts and readings from the G6 do not match symptoms or expectations or you’re taking over the recommended maximum dosage amount of 1000mg of acetaminophen every 6 hours, use a blood glucose meter to make diabetes treatment decisions. Seek medical advice and attention when appropriate, including for any medical emergency.
Failure to use the Dexcom G7 Continuous Glucose Monitoring System (G7) and its components according to the instructions for use provided with your device and available at https://www.dexcom.com/safety-information and to properly consider all indications, contraindications, warnings, precautions, and cautions in those instructions for use may result in you missing a severe hypoglycemia (low blood glucose) or hyperglycemia (high blood glucose) occurrence and/or making a treatment decision that may result in injury. If your glucose alerts and readings from the G7 do not match symptoms, use a blood glucose meter to make diabetes treatment decisions. Seek medical advice and attention when appropriate, including for any medical emergency.
